Base your code on the chief complaint and documentation, not assumptions about routine or medical visits. If it's a medical issue, use medical exam codes and link them to a precise ICD‑10 diagnosis.
The Essential Guide to Optometry Billing and Coding: What Every Practice Needs to Know (and Own!)

- Remove the current class from the content27_link item as Webflows native current state will automatically be applied.
- To add interactions which automatically expand and collapse sections in the table of contents select the content27_h-trigger element, add an element trigger and select Mouse click (tap)
- For the 1st click select the custom animation Content 27 table of contents [Expand] and for the 2nd click select the custom animation Content 27 table of contents [Collapse].
- In the Trigger Settings, deselect all checkboxes other than Desktop and above. This disables the interaction on tablet and below to prevent bugs when scrolling.
Prevent Denials, Survive Audits, and Catch Errors Before They Cost You
Billing is one of the most critical systems in any optometry practice. But it's also one of the easiest to get wrong. That's why every practice needs a reliable optometry billing and coding book to guide the process.
Coding errors can cost clinics up to $125,000 each year. Meanwhile, billing mistakes have led to losses of nearly $10,000 each month. That's more than $240,000 in annual revenue lost to preventable errors.
Yet, most teams are never formally trained in how to prevent medical billing mistakes. Even the most capable staff end up guessing when the process isn't clear.
Use this optometry coding and billing guide to stay consistent and avoid errors.
5 Popular Resources for Optometry Billing and Coding Books
Optometry codes come from several resources, each focused on a different part of the process. Bookmark the core references below that your team should use to for optometric billing and insurance claims.
1. ICD-10-CM Codes
Used for diagnosing conditions, ICD-10-CM codes must be specific to support reimbursement. Optometrists often reference codes for refractive errors, cataracts, and diabetic retinopathy.
2. CPT Codes
CPT codes document procedures like exams, tonometry, and imaging. Knowing which ones apply helps prevent underbilling.
3. HCPCS Level II Codes
Alphanumeric codes that cover supplies and equipment not included in CPT, such as contact lenses, medications, and durable medical equipment (DME). They're essential for billing vision-related supplies under Medicare and other payers.
4. Modifiers
Modifiers explain why a service was necessary. Common ones in optometry include:
- -25: Separate E/M service on the same day as another procedure
- -59: Distinct procedural service
5. LCDs & NCDs
Local and National Coverage Determinations define what Medicare covers. Learn your region’s LCDs to avoid denials.
Payer-Specific Rules
Every insurer sets its own policies for coverage, coding, and documentation. Some require prior authorization for procedures that others don't. Others deny claims based on the phrasing of a diagnosis.
That's why it's important to review your top payers' guidelines regularly. Treating them all the same leads to costly denials and extra work.
Benefits of a Go-to Guide
When your team knows which resources to rely on and how to use them, billing stays accurate and defensible. A reliable guide:
- Reduces claim rejections through accurate coding for billing services
- Prepares staff to handle audits with confidence
- Keeps documentation in line with payer rules
- Lowers the risk of penalties from billing errors
Coding Each Step of the Patient Journey
Every patient encounter creates a billing trail. Knowing which codes to use (and when) starts from the moment the patient walks in.
Initial Patient Visit
- Patient intake forms. Collect accurate insurance and demographic details upfront. Errors here often lead to claim rejections and eligibility issues.
- Verification of benefits. Confirm coverage before the visit. Check for exclusions, referral or authorization requirements, and patient responsibility like copays or deductibles.
- Chief complaint documentation. Link every complaint to a specific ICD-10 code. Avoid vague language; unclear documentation weakens your coding and reduces reimbursement odds.
- Exam codes (92000 vs. 99000 series). 92000 codes apply to routine or comprehensive eye exams. Use 99000 codes when the focus is medical, like evaluating an eye infection or managing chronic disease.
Special Tests and Procedures
Medical decisions for special tests and procedures require special attention from billers. Common tests like OCT (92133/92134), visual fields (92083), corneal topography (92025), and fundus photography (92250) must be linked to a diagnosis to support medical necessity.
Be aware of bundling rules. Some codes may not be reimbursed separately if performed on the same day as a comprehensive eye exam.
Medical vs. Routine Eye Exams
Always document whether the exam is medical (diagnosis-driven, often covered by health insurance) or routine (vision screening, typically covered by vision plans).
If a patient presents for a routine checkup but reports a medical issue—like dry eye, sudden vision changes, or eye pain—the visit may be billed as medical. Just make sure the documentation and diagnosis support the claim.
Refraction is usually coded with 92015 and is often considered non-covered. Be upfront with patients about potential out-of-pocket costs.
2 Common Modifiers
Used correctly, modifiers can help prevent denials and ensure accurate payment for eye care.

Common Pitfalls to Avoid When Managing Billing In-House
Managing billing internally can work well, but only if you avoid the missteps that often cost practices time and money.
- Under-coding or up-coding. Coding too low reduces revenue; coding too high can trigger audits. Accuracy is key.
- Missing documentation. If your notes don't fully support the codes used, payers will reject the claim.
- Overlooking payer rules. Each insurer has unique policies. Skipping these details leads to preventable denials.
- Falling behind on code updates. Codes change annually. Using outdated ones signals noncompliance and results in rejections.
- Skipping appeals. Denied claims should be reviewed, corrected, and resubmitted. Don’t leave money on the table.
- Poor handoff between clinical and billing teams. Even small miscommunications can lead to missing documentation or denied claims. Align on what needs to be documented and why.

Bring Your Billing In-House with RevolutionEHR
Billing and coding are too important to leave to chance. Without structure, even skilled teams can struggle to keep up. And when those gaps persist, they open the door to denials, audits, and lost revenue.
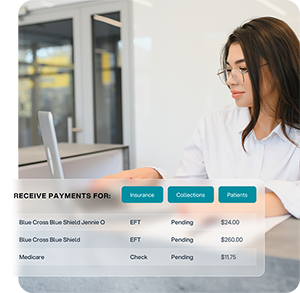
RevolutionEHR is an optometry EHR (electronic health record) that helps your practice take control of billing without adding extra burden. Its built-in clearinghouse, RevClear, accelerates claim submission and catches errors before they cost you. RevBilling backs you with expert support for coding, denials, and reconciliation.
Your team benefits with:
- Faster claims through built-in automation
- Fewer denials thanks to real-time tracking
- Easier resubmissions with guided corrections
- Hands-on help for appeals and coding accuracy
- Transparent dashboards to monitor performance
Curious how it all works in practice? Explore RevClear and RevBilling to see our optometry practice management software they support accurate claims, faster reimbursements, and fewer billing headaches.




